ACL Graft Selection & Early - Mid Stage Rehab: Considerations for the Rehab Professional
- Justin Richardson
- Jul 3, 2022
- 12 min read
Updated: Jul 7, 2022

When assessing the suitability of graft donor sites for athletes prior to ACL reconstruction (ACLr), there are many factors that may be considered in order to promote the most optimal outcome for the athlete. Factors such as graft stability, athlete sport / position and occupation (if not professional) are common amongst the decision making process, in line with the surgical preference of the orthopod, however little information exists on how to tailor rehabilitation towards different graft selections. This blog will outline some of the most common graft selections that are utilised in clinical practice, advantages & disadvantages associated with each selection and the clinical implications in early to middle stage rehabilitation associated with each.
Allograft vs Autograft
When making decisions regarding ACL graft choices, the first consideration is whether to utilise Allograft or Autograft tissue. Historically, Allograft tissue had traditionally been utilised in revision type ACLr scenarios or in individuals who had low pivoting demand due to evidence displaying poorer clinical outcomes when used in a primary settings (Cusumano et al 2022). However there is an increasing understanding, particularly around the restoration of athletic function in the role that donor site morbidity may play in the reduction of athletic performance. In addition, newer techniques of preservation have improved clinical outcomes related to Allograft tissue and thus these selections are improving in popularity for the primary ACL reconstruction.
Autografts remain the more simple process when it comes to predicting outcomes with the athlete as biologically, the tissue is more likely to be accepted by the body, there is higher predictability in tensile graft strength and the cost associated with graft harvesting and preservation is lower. If an autograft is chosen, typically the decision will be made between Bone-Patella Tendon-Bone (BPTB) or Semitendinosus-Gracilis (ST-G). This decision can be made based upon:
Athlete level of sport
Athlete sport of choice (& position within the sport)
Prior morbidity
Surgeon preference
Athlete occupation (amateur & semi pro)
In a generalist stand point, BPTB grafts are largely reserved for higher level athletes, who come from more running (& less jumping) based sports, have a higher background of quadricep muscle strength & mass and do not require kneeling for any occupation they may participate in outside of sport. ST-G grafts are then reserved for athletes who come from lower levels of sport, from more jumping based sports or aren't reliant on speed and have had no prior history of distal hamstring problems.
What makes an Allograft unique?
Common locations of an allograft include Tibialis anterior, Tibialis posterior, Achilles tendon, and BPTB allografts (Kaeding et al 2011). There is strong evidence to suggest that the tensile strength of allografts decreases with the age of the donor, with grafts donated from <30 year olds having significant higher strength than those >50 years old (Shelton et al 2021). Less common considerations that need to be accounted for with the allograft is whether they are sterilised using an irradiation or non-irradiation process (higher failure rates observed with irradiated processes) and preservation techniques with lower freeze-thaw numbers and time frozen associated with better outcomes (Lansdown et al 2017) (Kaeding et al 2011). With these variables in mind, there remains greater consistency in the preparation of autograft tissue due to it's close relationship with the biological donor.
Common Autografts: Bone-Patella Tendon-Bone & Semitendinosus-Gracillis
Currently, there is inconclusive evidence surrounding superior outcomes in the space of ACLr autografts. Recently, there has been scrutiny placed on the structural stability provided by ST-G autografts with as many as up to 40% displaying clinical failure and up to 11% experiencing graft re-rupture (Getgood et al 2020). This has been a key contributor to the rise in the use of the lateral extra-articular tenodesis which displays promising results in reducing re-rupture rates in high risk individuals (Getgood et al 2020). Historically, the BPTB autograft was the gold standard for ACLR, as it allowed proper bone-to-bone tunnel healing, involved a short fixation distance, and provided excellent biomechanical strength. (Zhao et al 2020). BPTB autografts have been criticised over the morbidity cost they present to anterior knee function during the rehabilitation process and in long term outcomes, with an increased risk of patellofemoral joint osteoarthritis identified in comparison to the ST-G autograft (Zhao et al 2020). Importantly for the rehabilitating clinician is to understand the difference between the two graft types and how to optimise rehabilitation in order to achieve best clinical outcomes.
Soft Tissue vs Bone to Bone Graft
The primary difference between the soft tissue and bone to bone graft type is positioned in the physiology of the placement in their respective tunnels and the histological remodelling that occurs. In the ACLr graft tissue the following phases of healing occur:
Early Healing Phase
Defined until the fourth postoperative week, marked by increasing necrosis at the centre of the graft with no revascularisation. As this gradual process occurs, the mechanical tensile strength of the graft slowly decreases and there is a lack of sufficient biological graft incorporation at the bony tunnel sites.
Proliferation Phase
Defined as the period between weeks 4-12 post operatively, whereby an increase in graft necrosis occurs followed by a process of revascularisation. It is believed that the graft is at its weakest in weeks 6-8 whereby an increase in type 3 collagen (in comparison to type 1 collagen) leads to a lower stress-strain failure point. Clinicians should be aware that loading must be sufficient enough to stimulate cellular and extra-cellular changes for preservation of graft stability whilst not overloading the graft that may lead to increased stretch of the tissue.
Ligamentisation Phase
Defined as the period from week 12 onwards, this is characterised by a slow revascularisation of the graft tissue until it reaches levels similar to that of the native ACL at ~6 months post operatively. Importantly, the heterogenous composition of collagen fibres that is seen in the intact ACL is never truely restored and that the mechanical properties of the reconstructed ACL reach their peak function at ~1 year post op.
Figure 1 - Healing phases of ACL graft tissue
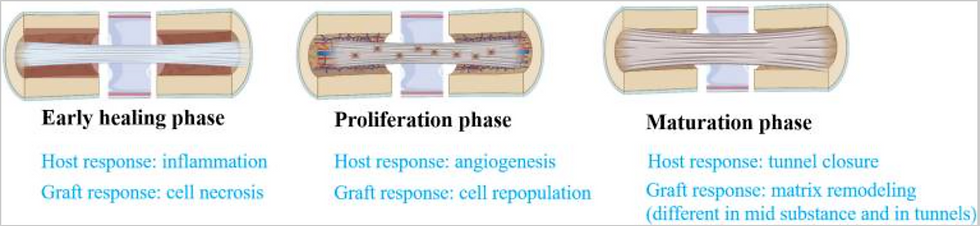
Figure 2 - Healing Phases of ACL Graft Tissue

Tunnel Site Healing: An important differential
Tendon to Bone healing is a fundamental concern associated with the hamstring tendon autograft. Tendon-to-bone healing in a bone tunnel occurs by bone ingrowth into the fibrovascular interface tissue that initially forms between the tendon and the bone. First, progressive mineralization of the interface tissue occurs. Subsequently, the bone grows into the outer tendon and the tendon graft becomes incorporated into the surrounding bone. Progressive re-establishment of the continuity of collagen fibers between the tendon and the bone results in restoration of a tendon-bone junction (Chen et al 2009). For the treating clinician, understanding the physiology and fragility behind this process can assist in the prescription of Closed & Open Kinetic Chain loading (CKC & OKC), and it's respective implications on the tunnel sites, indicating that exercises that promote less ACL & anterior tibial translation loading may be implicated during the first 6-8 weeks postoperatively as the tunnel sites begin to fuse (Escamilla et al 2012).
Contrastingly, with the BPTB graft, as there is the presence of a bone-bone plug within the tunnel insertion sites, a more secure fixation can be identified (Zein et al 2017). This fixation, allows the most physiological reconstruction because of the natural insertion site of tendon being preserved on the bone plug and a stronger acceptance within the tunnel sites. Clinically this provides a platform for the treating clinician to be far more aggressive in their early rehabilitation approach.
Clinical Advantages:
When assessing the clinical advantages of each graft selection, it can be apparent that the primary advantage of an allograft surrounds it's lack of donor site morbidity, the increased graft type and variability as well as accelerated post operative function. The primary argument for a hamstring tendon autograft is that it has a high load to failure in comparison with an allograft, provides less morbidity than a BPTB graft and is an easier operation technically to perform. Structurally, the BPTB graft allows for the greatest like for like function with the natural ACL, provides a strong bone-bone plug and produces outstanding long term stability outcomes.
Clinical Disadvantages:
When analysing the clinical disadvantages of each graft tissue, there is concern over the long term function of allograft tissue along with a higher risk of infection, lower tensile strength and inconsistency with body rejection of the graft. Hamstring tendon autografts produce high levels of hamstring morbidity, which is an emerging area of research for the protection of grafts in pivoting sports. The primary concern with BPTB autografts exists around the presence of anterior knee morbidity and quadricep weakness post operatively.
Implications for Rehabilitation: What the clinician needs to know
It is important to consider that whilst end stage rehab should remain similar, regardless of which graft tissue type is used; there is deviation that exists in the early stages of rehabilitation that will build strong foundations for success in late stage rehab.
Recommendations for Early Stage Rehab:
Allograft
Despite clinical athlete morbidity, restrict loads that place high tensile strength on the ACL tunnel sites and high Tibiofemoral & Patellofemoral loads within the early healing phase and early proliferation phase of graft acceptance.
Hamstring Tendon
An initial period of reduced distal hamstring loading is recommended to ensure optimal scarring and collagen reformation at the site of the ST-G muscle-tendon lesion that is used for the graft site. This period should be ~2-3 weeks and following then, a G4 Tendon lesion like rehabilitation journey should occur for the hamstring muscle group. This would ideally focus on concentric inner range --> Isometric Mid Range --> Concentric Outer Range --> Isometric Outer Range --> Eccentric Loading. For quadricep loading patterns, caution should be present over loading strategies that provide increase ACL and tunnel site tensile load within the first 6-8 weeks as tendon-bone healing occurs.
Figure 3 - Example Week 1 post ACLR Hamstring Donor Site Conditioning

Figure 4 - Example Weeks 2-3 post ACLR Hamstring Donor Site Conditioning

BPTB
As a large energy storage-release tendon like lesion has occurred within the harvesting of the graft. Principles of tendon proliferation should be adhered to with a high focus on maximal voluntary isometric quad contraction followed by heavy, slow isotonic resistance training. Patellofemoral de-loading strategies should be administered in order to reduce compression and stretch over the healing tendon site. Restoration of neuromuscular activation should occur in smaller degrees of knee flexion first before shifting to greater degrees of knee flexion.
Figure 5 - Example Weeks 1 post ACLR BPTB Donor Site Conditioning

Figure 6 - Example Weeks 2-3 post ACLR BPTB Donor Site Conditioning

Recommendations for Mid Stage Rehab:
Allograft
Whilst allograft tissue provides no donor site morbidity, the relevant implications of the proliferation and early ligamentisation phase of graft healing are positioned in the tibio-femoral joints ability to tolerate ground reaction force. In the mid stages of rehabilitation, a primary objective for the treating clinician is to implement an effective return to run strategy. Careful considerations should be made when implementing a return to run program and concurrently implementing the early stages of the plyometric continuum. Effectively periodising ground reaction loading should allow adequate (at least 36hrs) recovery time between bouts of intensive plyometric loads. As the joint accepts and tolerates this stimulus this can be reduced to an ~24 hour window. If the treating clinician has accessibility to modified surface modalities (Airtrack, Mini Tramp, Alter G), these can be utilised in order to reduce ground reaction forces whilst still promoting stretch shortening cycle development.
Figure 7 - Example Weekly Periodisation Mid Stage Post ACLR

Hamstring Graft
As the tunnel sites ossify and the graft begins it's process of ligamentisation, attention can be drawn towards increasing the intensity of patellofemoral & tibiofemoral joint loading*. Morbidity surrounding the hamstring donor site can be identified as a large source of dysfunction for the athlete with altered gait patterns commonly present due to the loss of semitendinosus function. Once initial type 3 collagen has been laid, the objective of donor site conditioning should be on transitioning this to type 1 collagen and increasing positive tendon adaptations. Foundations of isometric and inner range concentric rehabilitation should be progressed towards maximal overcoming and yielding based isometrics along with eccentric loading. The objective of eccentric loading is centred around the neuromuscular innervation of the semitendinosus and increasing the fascicle length of the long head of Biceps Femoris which appears to present with shorter fascicle lengths and increased pennation angles post ACLr. Recruitment of the medial hamstrings during hip dominant movement patterns should be considered and exercise prescription should be geared around monitoring movement strategies of the athlete. Common compensation patterns include increased lateral foot rotation during gait and unilateral exercises which not only decreases medial hamstring function but also places the lateral rotators of the hip in a shortened position, reducing their effectiveness at controlling dynamic knee valgus.
*Based upon present of concomitant injuries...
Figure 8 - Example Weeks 4-7 Hamstring Graft Donor Site Conditioning

Figure 9 - Example Weeks 8-10 Hamstring Graft Donor Site Conditioning

BPTB Graft
Once initial foundations of neuromuscular activation and range of motion have been laid, the primary objective for the BPTB graft is to elicit positive tendon morphology adaptations. Increased tendon cross-sectional area will assist the athlete in withstanding heavier loads that are required in order to develop adequate quadriceps hypertrophy. Key principles involved with this process is to begin tendon development in positions that place the patella tendon under the smallest amounts of compression and stretch during early stages of development before gradually increasing eccentric demand on the tendon. Practically speaking this will mean that practitioners are loading athletes heavier in positions of relative knee extension and shift them towards positions of increased knee flexion as quadricep bulk, tendon capacity and pain allows. From a framework standpoint, practitioners should aim to develop heavier loads, under increased time under tension in shorter ranges of motion before shifting towards larger ranges of motion. This challenges a traditional dogma whereby typically in rehabilitation we will aim to load athletes under full range before increasing external loads placed upon them.
Figure 10 - Example Weeks 4-7 BPTB Graft Donor Site Conditioning

Figure 11 - Example Weeks 8-10 BPTB Graft Donor Site Conditioning

Principles of Donor Site Development
Whilst the physiology of graft healing and donor site morbidity may appear to be a complicated beast, it is important to maintain a broad principles based approach towards program design. Within both the contexts of hamstring and BPTB grafts it is plausible to believe that self limiting isometric contractions in shallow ranges lay a foundation for tendon restoration before utilising a graded approach to concentric and eccentric contractions.
Below is an example framework for development within the first three months of rehabilitation and what may be some key focus areas for the rehabilitating clinician. It is important to consider that all athletes are individuals and based on their training age, concomitant injuries and technical proficiency will progress at individual rates.
Figure 12 - Example Hamstring Graft Donor Site Development Framework

Figure 13 - Example BPTB Graft Donor Site Development Framework

Conclusion
ACL graft selection should be individualised based upon numerous factors surrounding an athletes sport of choice, prior injury history & tissue morphology. For the rehabilitation professional, program considerations should concern the ability of the graft of choice to be accepted within the tibial and femoral tunnels and the rehabilitation of the relevant donor site. Whilst no donor site morbidity is present, Allografts present the challenge of delayed acceptance within the body which may present challenges of persistent effusions. Hamstring graft tendons are a soft tissue to bone graft which allows a slower tunnel site healing process, along with the donor site location lay a platform for more cautious protection phases. BPTB grafts being a bone to bone graft allow the clinician to perform early vigorous rehabilitation, however present challenges in the restoration of tendon cross section area within the patella tendon and tolerance of load through the patellofemoral joint.
Developing a framework for rehabilitation is pivotal in allowing a scalable approach to athletic development post ACL reconstruction. Above are displayed some examples of how a clinician might transition an athlete through early to mid stage rehabilitation. If you are a rehab professional who is aiming to develop a systemised approach to ACL rehabilitation, the Athletes Authority ACL Mentorship process allows you the freedom to be able to have a road map of progression throughout the 5 phases of rehabilitation, whilst granting you the freedom to individualise specifics of your program to the athlete in front of you.
Applications are open for our September intake, I hope to see you there
https://athletesauthority.education/acl-mentorship/
Yours in Rehab
JR
References
Cusumano, A., Capitani, P., Messina, C. et al. Different timing in allograft and autograft maturation after primary anterior cruciate ligament reconstruction does not influence the clinical outcome at mid-long-term follow-up. Knee Surg Sports Traumatol Arthrosc30, 2281–2290 (2022). https://doi.org/10.1007/s00167-021-06785-4
Kaeding, C. C., Aros, B., Pedroza, A., Pifel, E., Amendola, A., Andrish, J. T., Dunn, W. R., Marx, R. G., McCarty, E. C., Parker, R. D., Wright, R. W., & Spindler, K. P. (2011). Allograft Versus Autograft Anterior Cruciate Ligament Reconstruction: Predictors of Failure From a MOON Prospective Longitudinal Cohort. Sports health, 3(1), 73–81. https://doi.org/10.1177/1941738110386185
Trevor J. Shelton, Connor Delman, Sean McNary, J. Ryan Taylor, Richard A. Marder,
Aging Decreases the Ultimate Tensile Strength of Bone–Patellar Tendon–Bone Allografts,
Arthroscopy: The Journal of Arthroscopic & Related Surgery,
Volume 37, Issue 7, 2021, Pages 2173-2180, ISSN 0749-8063,
Lansdown, D. A., Riff, A. J., Meadows, M., Yanke, A. B., & Bach, B. R., Jr (2017). What Factors Influence the Biomechanical Properties of Allograft Tissue for ACL Reconstruction? A Systematic Review. Clinical orthopaedics and related research, 475(10), 2412–2426. https://doi.org/10.1007/s11999-017-5330-9
Getgood, A., Bryant, D. M., Litchfield, R., Heard, M., McCormack, R. G., Rezansoff, A., Peterson, D., Bardana, D., MacDonald, P. B., Verdonk, P., Spalding, T., STABILITY Study Group, Willits, K., Birmingham, T., Hewison, C., Wanlin, S., Firth, A., Pinto, R., Martindale, A., O'Neill, L., … Van Haver, M. (2020). Lateral Extra-articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes From the STABILITY Study Randomized Clinical Trial. The American journal of sports medicine, 48(2), 285–297. https://doi.org/10.1177/0363546519896333
Zhao, L., Lu, M., Deng, M., Xing, J., He, L., & Wang, C. (2020). Outcome of bone-patellar tendon-bone vs hamstring tendon autograft for anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials with a 5-year minimum follow-up. Medicine, 99(48), e23476. https://doi.org/10.1097/MD.0000000000023476
Chen C. H. (2009). Graft healing in anterior cruciate ligament reconstruction. Sports medicine, arthroscopy, rehabilitation, therapy & technology : SMARTT, 1(1), 21. https://doi.org/10.1186/1758-2555-1-21
Escamilla, R. F., Macleod, T. D., Wilk, K. E., Paulos, L., & Andrews, J. R. (2012). Anterior cruciate ligament strain and tensile forces for weight-bearing and non-weight-bearing exercises: a guide to exercise selection. The Journal of orthopaedic and sports physical therapy, 42(3), 208–220. https://doi.org/10.2519/jospt.2012.3768
Zein, A., Ali, M., Zenhom Mahmoud, A., & Omran, K. (2017). Autogenous Hamstring-Bone Graft Preparation for Anterior Cruciate Ligament Reconstruction. Arthroscopy techniques, 6(4), e1253–e1262. https://doi.org/10.1016/j.eats.2017.04.011
.png)






Comments